Fixed partial dentures, commonly known as dental bridges, are prosthetic devices used to replace one or more missing teeth. Unlike removable partial dentures, which can be taken out and cleaned daily, fixed partial dentures are cemented onto existing teeth or dental implants and are not removable by the patient. These bridges help restore the natural function and appearance of teeth, providing a stable and permanent solution to tooth loss.
Who Needs Fixed Partial Dentures?
Fixed partial dentures are primarily indicated for individuals who have one or more missing teeth but still retain healthy teeth on either side of the gap. Here are some specific scenarios where fixed partial dentures are recommended:
- Single or Multiple Tooth Loss: Patients who have lost one or several teeth due to decay, injury, or periodontal disease.
- Healthy Adjacent Teeth: Candidates must have strong, healthy teeth (abutment teeth) on either side of the missing tooth or teeth to support the bridge.
- Desire for a Permanent Solution: Individuals who prefer a fixed, non-removable solution over removable partial dentures.
- Good Oral Hygiene: Suitable candidates must be committed to maintaining good oral hygiene to ensure the longevity of the fixed partial dentures.
Components of Fixed Partial Dentures
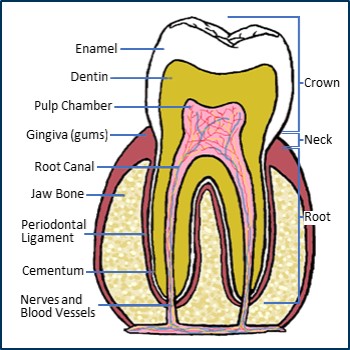
- Abutment Teeth: These are the natural teeth or implants on either side of the gap left by missing teeth. They act as anchors for the bridge.
- Pontics: The false teeth that replace the missing ones. They are connected to the crowns on the abutment teeth and fill in the gap.
- Crowns: These cover the abutment teeth to provide support for the pontics. Crowns are made to match the natural teeth in color and shape.
Types of Fixed Partial Dentures



- Traditional Fixed Bridges: These are the most common type, consisting of one or more pontics held in place by dental crowns on the abutment teeth. They are typically used when natural teeth are present on both sides of the gap.
- Cantilever Bridges: These are used when there is only one adjacent tooth next to the gap. The pontic is anchored to one or more abutment teeth on one side.
- Resin-Bonded Bridges (Maryland Bridges): These are less invasive and involve bonding a metal or porcelain framework to the back of adjacent teeth, with a pontic in the middle. They are often used for missing front teeth.
Benefits of Fixed Partial Dentures
- Improved Aesthetics: They restore the natural appearance of the smile by filling in gaps left by missing teeth.
- Enhanced Functionality: They enable better chewing and speaking compared to having missing teeth.
- Preservation of Adjacent Teeth: By filling the gap, they prevent the remaining teeth from shifting out of place, which can lead to bite issues and further tooth loss.
- Durability and Stability: Fixed partial dentures are designed to be long-lasting and stable, providing a permanent solution compared to removable options.
- Boost in Self-Confidence: Replacing missing teeth with fixed partial dentures can significantly improve a person’s self-esteem and overall quality of life.
Assessing Suitability
A thorough dental examination and consultation are essential to assess a patient’s suitability for fixed partial dentures. This includes:
- Dental History and Examination: Review of the patient’s dental and medical history, along with a detailed examination of the oral cavity.
- Diagnostic Imaging: X-rays and, in some cases, CT scans to evaluate bone density and the condition of abutment teeth.
- Treatment Planning: Customized treatment planning based on the patient’s specific needs, health status, and personal preferences.
By considering these factors, dentists can determine the best course of action to restore a patient’s smile and oral function, ensuring that fixed partial dentures are a viable and effective option.
Alternatives of Fixed Partial Dentures
For patients who are not suitable for fixed partial dentures, several alternative dental solutions can be considered:
- Removable Partial Dentures: These are suitable for patients who cannot have fixed partial dentures due to gum disease or bone loss. Removable partial dentures can be taken out and cleaned daily.
- Dental Implants: For those with sufficient bone density, dental implants can provide a stable and permanent solution without relying on adjacent teeth.
- Full Dentures: In cases of extensive tooth loss, full dentures may be the best option, especially when most or all teeth are missing in an arch.
- Implant-Supported Bridges: For patients with multiple missing teeth and adequate bone structure, implant-supported bridges offer a fixed solution that does not depend on natural teeth for support.
The Procedure for Getting Fixed Partial Dentures
1. Initial Consultation and Examination
The journey to receiving fixed partial dentures begins with a thorough consultation and examination:
- Medical and Dental History: The dentist will review your medical and dental history to identify any conditions that might affect the treatment.
- Oral Examination: A comprehensive examination of your mouth, including teeth, gums, and jawbone, is conducted.
- Diagnostic Imaging: X-rays, and sometimes CT scans, are taken to assess the health and structure of your teeth and jawbone, and to plan the placement of the fixed partial denture.
2. Treatment Planning and Design
After the initial consultation, a customized treatment plan is developed:
- Treatment Discussion: The dentist discusses the findings and presents the best treatment options, including the type of fixed partial denture suitable for your needs.
- Designing the Denture: Impressions of your teeth are taken to create a model. This helps in designing a denture that fits perfectly and looks natural.
- Shade Matching: The color of the pontics (artificial teeth) is matched to your natural teeth for a seamless appearance.
3. Tooth Preparation and Impression Taking
Preparing the abutment teeth (teeth adjacent to the gap) is a crucial step:
- Anesthesia: Local anesthesia is administered to numb the area and ensure comfort during the procedure.
- Tooth Shaping: The abutment teeth are reshaped to accommodate the crowns that will support the bridge. This involves removing a small portion of enamel from these teeth.
- Impressions: Detailed impressions of the prepared teeth and the surrounding area are taken. These impressions are sent to a dental lab to fabricate the fixed partial denture.
4. Temporary Dentures and Waiting Period
While the permanent fixed partial denture is being crafted, temporary dentures are placed:
- Placement of Temporary Bridge: A temporary bridge is fitted to protect the prepared teeth and maintain aesthetics and function.
- Waiting Period: This period typically lasts a few weeks while the permanent denture is made. During this time, it’s important to follow the dentist’s instructions on care and maintenance of the temporary bridge.
5. Final Placement and Fitting
Once the permanent fixed partial denture is ready, the final placement procedure is carried out:
- Removal of Temporary Bridge: The temporary bridge is removed, and the area is cleaned.
- Checking the Fit: The dentist places the permanent fixed partial denture and checks the fit, making any necessary adjustments.
- Bonding: The denture is permanently cemented onto the abutment teeth. The dentist ensures that it fits comfortably and functions properly.
- Final Adjustments: Any minor adjustments needed for a perfect fit and optimal bite are made.
6. Follow-Up and Care
After the placement of the fixed partial denture, follow-up care is essential to ensure long-term success:
- Initial Follow-Up: A follow-up appointment is scheduled to check the fit and function of the denture, and to address any issues or discomfort.
- Regular Dental Check-Ups: Routine check-ups are crucial to monitor the condition of the fixed partial denture and the health of the surrounding teeth and gums.
- Oral Hygiene Practices: Maintaining excellent oral hygiene is critical. This includes brushing twice a day, flossing daily, and using interdental cleaners to remove plaque from around the denture.
- Dietary Recommendations: Follow any dietary guidelines provided by your dentist to avoid damaging the fixed partial denture.
Conclusion
Fixed partial dentures offer a reliable and aesthetically pleasing solution for individuals with missing teeth, enhancing both functionality and appearance. This comprehensive guide has covered everything you need to know about fixed partial dentures, from understanding their purpose and benefits to the detailed procedure involved in getting them.
The journey to obtaining fixed partial dentures involves careful planning, precise execution, and diligent follow-up care. By working closely with your dentist and committing to good oral hygiene practices, you can enjoy the long-lasting benefits of fixed partial dentures. If you’re considering this option, consult with a dental professional to determine the best course of action for your dental health.