Facing the prospect of wisdom tooth removal can be a daunting experience for many. Whether it’s the fear of the unknown, concerns about pain, or simply the idea of undergoing a surgical procedure, it’s natural to feel apprehensive. But understanding what to expect can go a long way in easing those worries. By the end of article, you’ll know exactly what to anticipate, helping you prepare mentally and physically for a smooth and successful experience.
Why Wisdom Teeth Removal is required
Understanding Wisdom Teeth
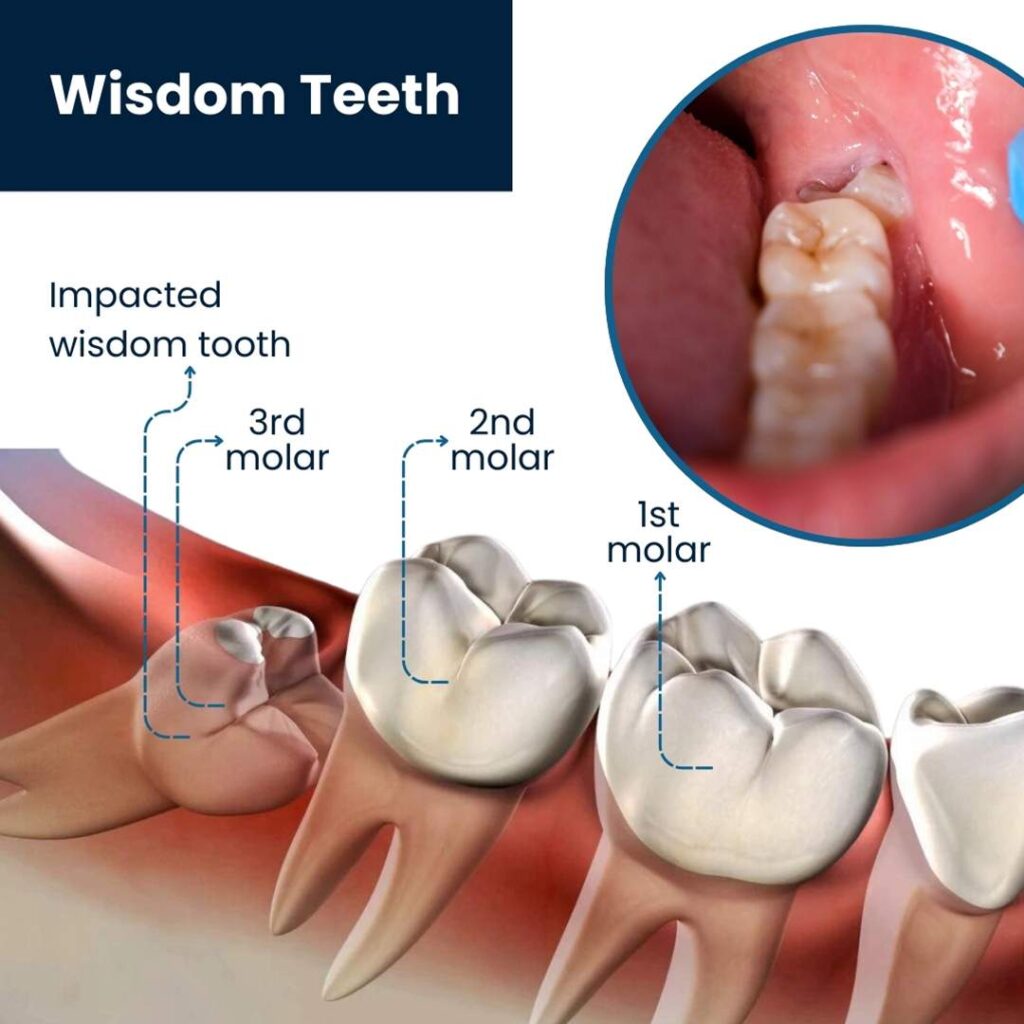
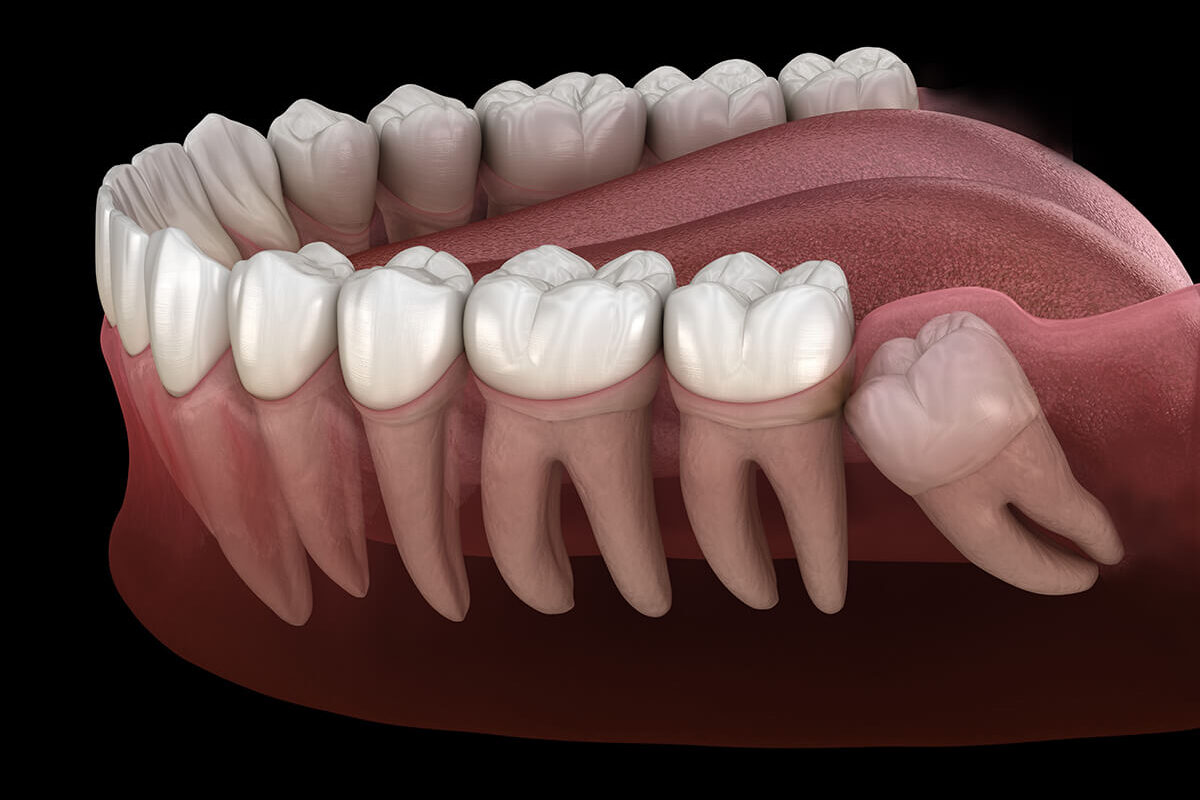
Wisdom teeth, also known as third molars, are the last set of teeth to develop, typically emerging in the late teens or early twenties. While these teeth were essential for our ancestors who needed extra molars to chew coarse, rough food like roots, nuts, and raw meat, they are often not necessary in modern diets. Additionally, the human jaw has evolved to become smaller over time, which means there often isn’t enough space to accommodate these extra teeth.
Common Issues Caused by Wisdom Teeth
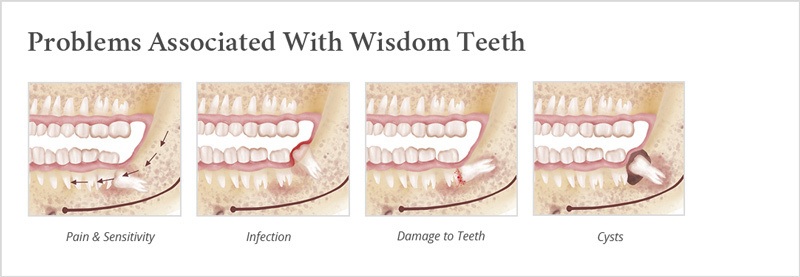
When wisdom teeth begin to emerge, they can cause a variety of problems, especially if there isn’t enough room for them to grow properly. These issues include:
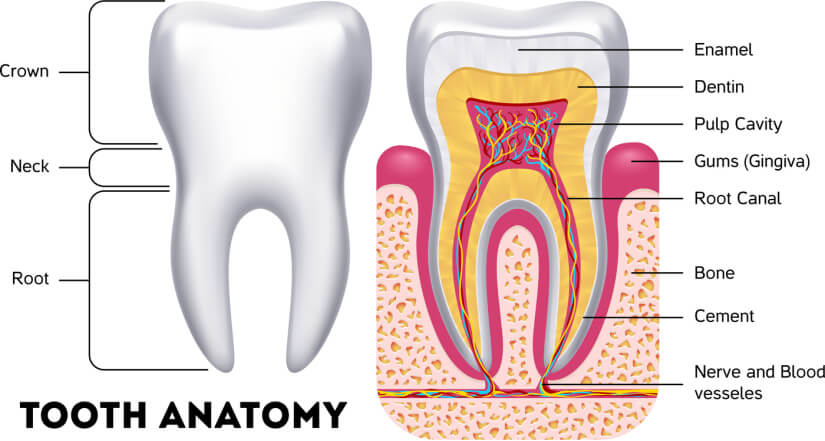
- Impaction: When wisdom teeth are trapped beneath the gums or within the jawbone, they are considered impacted. Impacted wisdom teeth can cause pain, swelling, and infections as they press against other teeth or damage the jawbone.
- Crowding: Even if wisdom teeth do emerge, they often do so at odd angles, leading to crowding and misalignment of the other teeth. This can undo years of orthodontic work and cause discomfort or difficulties with oral hygiene.
- Infections and Cavities: Partially erupted wisdom teeth are particularly prone to infections because they are difficult to clean properly. Food and bacteria can easily get trapped around them, leading to gum disease and cavities that can affect adjacent teeth.
- Cysts and Tumors: In rare cases, an impacted wisdom tooth can lead to the development of cysts or tumors in the jawbone, which can cause significant damage to the surrounding bone and tissues.
Wisdom Teeth Removal – What to expect during the procedure
Before the surgery, you’ll have a brief discussion with your oral surgeon. They’ll review the procedure one last time, answer any last-minute questions you might have, and ensure that you’re comfortable and ready. This is also when the surgeon will confirm the type of anesthesia to be used based on your pre-surgery consultation.
The Extraction Process
Once the anesthesia takes effect, the oral surgeon will begin the extraction process. The specific steps can vary depending on whether the teeth are impacted or fully erupted, but the general procedure is as follows:
- Incision and Access: For impacted wisdom teeth that haven’t fully emerged, the surgeon will start by making a small incision in the gum tissue to expose the tooth and surrounding bone. If necessary, a small portion of the bone covering the tooth may be removed to gain better access.
- Tooth Sectioning: In some cases, particularly with deeply impacted teeth, the surgeon may need to divide the tooth into smaller pieces. This technique allows for easier removal and minimizes the amount of bone that needs to be removed.
- Extraction: The tooth or its sections are gently rocked back and forth to loosen it from the socket before being lifted out with dental instruments. During this process, you might feel pressure but should not experience pain.
- Closing the Surgical Site: After the tooth is removed, the surgeon will clean the extraction site and may smooth out any rough bone edges. If an incision was made, it will be stitched closed with dissolvable or non-dissolvable sutures. A piece of gauze is then placed over the extraction site to help control bleeding and promote clot formation.
What You May Experience During the Procedure
While the surgery itself is generally straightforward, knowing what to expect during the procedure can help reduce anxiety:
- Sensation of Pressure: Even with anesthesia, it’s normal to feel some pressure as the surgeon works to remove the tooth. This is because the anesthesia numbs pain but doesn’t eliminate the sensation of movement.
- Sounds: You might hear some sounds during the procedure, such as the drill or the cracking of the tooth. These sounds are perfectly normal, though they can be unsettling. Many patients find comfort in focusing on their breathing or listening to calming music if allowed.
- Minimal Pain: Thanks to the anesthesia, you should not feel any pain during the extraction. If at any point you do experience discomfort, you can communicate this to your surgeon, who can administer additional anesthesia if needed.
Common Concerns and Questions regarding Wisdom Teeth Removal
Undergoing wisdom tooth removal can raise a lot of questions and concerns, especially if it’s your first time having a surgical dental procedure. This section addresses some of the most common worries patients have before and after the surgery, helping you feel more informed and reassured.
1. How Painful Will the Procedure Be?
One of the most common concerns is the level of pain associated with wisdom tooth removal. Here’s what you need to know:
- During the Surgery: With modern anesthesia options, you should not feel pain during the procedure. Local anesthesia will numb the area around your wisdom teeth, so while you may feel some pressure, there should be no sharp pain. If you’re particularly anxious or if the extraction is complex, sedation or general anesthesia can be used to ensure that you’re comfortable and pain-free throughout the surgery.
- After the Surgery: Post-operative pain is common, but it’s usually manageable with prescribed pain medications or over-the-counter options like ibuprofen. The intensity of pain varies depending on factors such as the complexity of the extraction and your pain tolerance, but it typically peaks within the first 24-48 hours and then gradually subsides over the next few days.
2. How Long Will It Take to Recover?
Recovery time can vary depending on the individual and the complexity of the surgery:
- Initial Recovery: Most patients start to feel better within 3-4 days after the surgery, although some swelling and mild discomfort can persist for up to a week.
- Full Recovery: Complete healing of the extraction site can take several weeks to a few months. During this time, the tissue will regenerate, and any jaw stiffness or soreness should resolve.
- Activity Resumption: You can usually return to light activities within a few days, but it’s recommended to avoid strenuous exercise or heavy lifting for at least a week to prevent complications like increased bleeding or dry socket.
3. Will I Need Stitches, and When Will They Be Removed?
Whether you need stitches depends on the complexity of your extraction:
- Types of Stitches: Some wisdom tooth extractions require stitches to close the incision site, particularly if the tooth was impacted or if a large incision was needed. Your oral surgeon may use either dissolvable stitches, which typically dissolve on their own within 7-10 days, or non-dissolvable stitches, which will need to be removed at a follow-up appointment.
- Stitch Care: If you have stitches, avoid touching them with your tongue or fingers, and follow your surgeon’s advice on keeping the area clean. If a stitch comes loose or causes discomfort, contact your surgeon.
4. Can I Eat Normally After the Surgery?
Your diet will need to be modified during the initial recovery period:
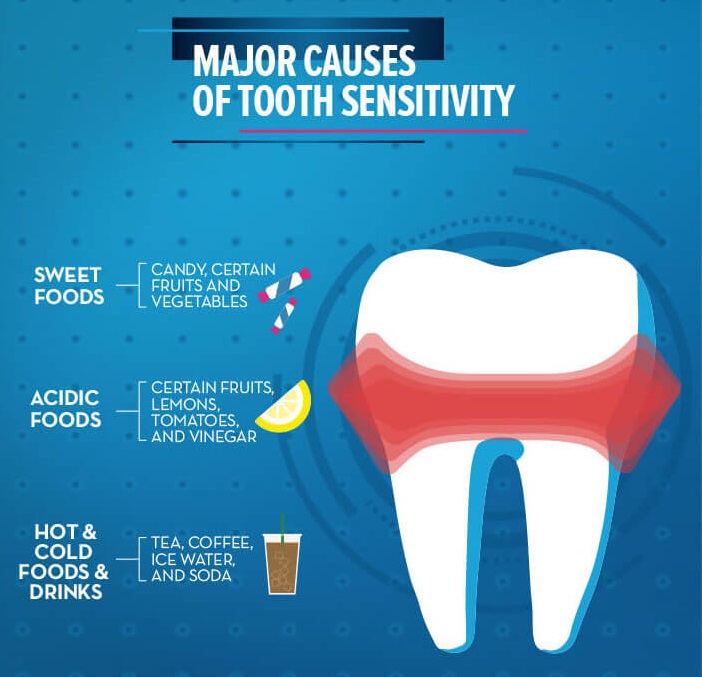
- First 24-48 Hours: Stick to soft, easy-to-swallow foods that don’t require much chewing, such as yogurt, applesauce, mashed potatoes, smoothies, and soup (cooled to lukewarm). Avoid hot, spicy, or crunchy foods that can irritate the extraction site.
- Gradual Reintroduction of Solid Foods: As your mouth heals, you can gradually reintroduce more solid foods. Chew on the opposite side of your mouth and avoid hard or sticky foods until you’re fully healed.
- Hydration: Staying hydrated is important, but avoid using straws, as the suction can disrupt the healing process.
5. When Should I Contact My Oral Surgeon?
It’s important to know when to reach out to your oral surgeon if you experience any post-surgery concerns:
- Severe Pain: While some discomfort is normal, severe pain that isn’t relieved by pain medication or that increases after a few days could indicate a complication like dry socket or infection.
- Excessive Bleeding: Some bleeding is normal within the first few hours, but if bleeding persists or is heavy, contact your surgeon.
- Fever or Signs of Infection: A fever, foul-smelling breath, or swelling that worsens after a few days could be signs of an infection and should be addressed promptly.
- Unusual Swelling or Bruising: Swelling and bruising are common, but if they’re extreme or don’t start to improve after a few days, it’s worth getting checked out.
Conclusion
Wisdom tooth removal is a common procedure that, while often necessary, can bring about a lot of anxiety and uncertainty. Understanding each step of the process—from why wisdom teeth are removed, to what happens during the surgery, to the recovery that follows—can help alleviate some of that stress. By being informed and prepared, you can approach your wisdom tooth extraction with confidence, knowing what to expect and how to manage your recovery effectively. Remember, every individual’s experience is unique, but with the right preparation and aftercare, you can ensure a smoother, more comfortable recovery. Whether you’re scheduling your procedure or supporting someone through theirs, this guide provides the knowledge you need to navigate wisdom tooth removal with ease.